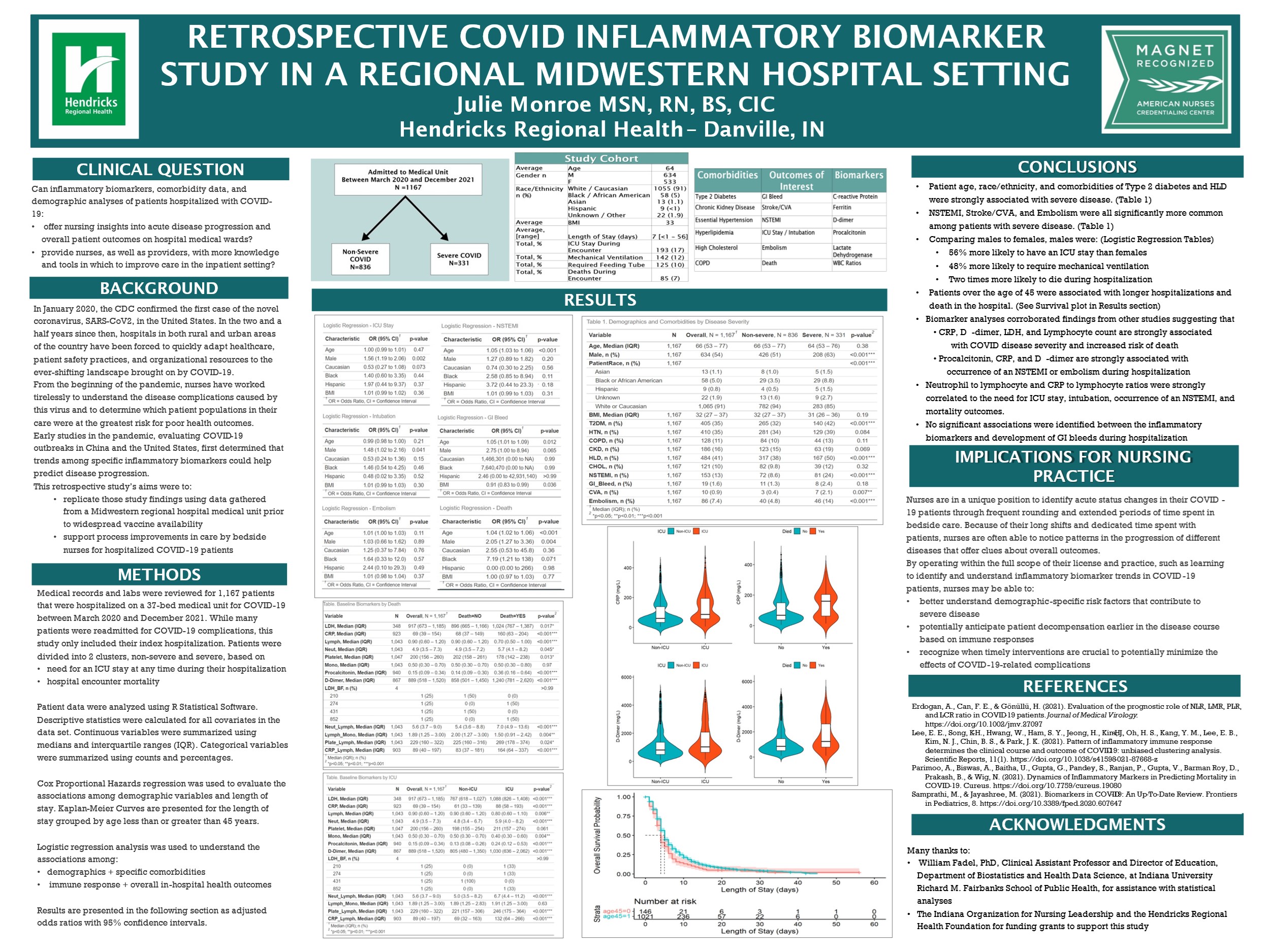
The purpose of this study was to both further nursing research in this hospital setting as well as to foster process improvement in nursing care for COVID-19 patients. Julie Monroe, MSN, RN, BS, CIC, Hendricks Regional Health Infection Preventionist, and William Fadel, PhD, Indiana University Richard M. Fairbanks School of Public Health and School of Medicine Clinical Assistant Professor, collected data on approximately 1,150 patients who were hospitalized between March 2020 and November 2021. Labs of interest, as identified through relevant COVID-19 research scientific literature, included: procalcitonin, d-dimer, ferritin, lactate dehydrogenase, C-reactive protein, and absolute monocyte, lymphocyte, and neutrophil ratios. Patient comorbidities of interest include Type 2 diabetes, hypertension, hyperlipidemia, high cholesterol, and chronic kidney disease. Patient demographics that were evaluated include race/ethnicity, gender, age, and BMI. Hospitalization outcomes included the need for an ICU stay, need for ventilation, NSTEMI, stroke/embolism, GI bleed, and death.
These demographics, labs, and hospitalization outcomes were analyzed through descriptive statistics and regression analysis to identify specific acute outcomes among COVID-19 patients and any significant correlations between these variables.
Outcomes of the study, based on our specific population (unvaccinated or only partially vaccinated patients, first COVID hospitalization):
Males are:
1. Just over 50% more likely to have a COVID-related ICU stay compared to females
2. Just under 50% more likely to require ventilation during a COVID-related hospital stay than females
3. Twice as likely to die during hospitalization for COVID
Patients over the age of 45 are:
1. More likely to have longer hospital stays
2. More likely to experience an NSTEMI related to COVID
3. More likely to die during hospitalization
Patient age and race/ethnicity, with comorbidities of Type 2 diabetes and HLD, were strongly associated with severe COVID-19 disease.
 *This project was funded by a grant provided by the Hendricks Regional Health Foundation.
*This project was funded by a grant provided by the Hendricks Regional Health Foundation.